What’s the Difference Between Medical Coding & Medical Billing?
Medical billing and medical coding are vital jobs that help keep hospitals and doctor’s offices running. They work behind the scenes ensuring patients, hospitals, and insurance companies receive the correct information and bills. Sometimes, these roles are combined into a single position. However, many hospitals still hire separate billers and coders to ensure quality work.
Indeed, these jobs require accuracy, speed, and a keen eye for detail. Mistakes could result in delayed or incorrect payments. They may even result in a patient’s claim being denied by insurance, which can be devastating.
Some employers choose to combine the roles due to how they interact. Indeed, billing and coding work as a baton toss. Notably, coders turn charts and patient information into codes. These codes make it easier for individual hospitals and insurance providers to communicate with each other. Consider how many different ways a doctor may look at symptoms, plan treatment paths, or simply word their notes on a chart. By translating these reports into universal codes, insurers and billers can read charts more easily.
Once coders have translated reports into code, billers take over. They create invoices, bills, and claims using the coder’s data. From there, billers oversee the billing and payment process, which may include correcting mistakes.
Keep reading to learn more about the differences between medical billing and medical coding.
Medical Coding
Your chart will go to a medical coder whenever you visit a hospital or doctor’s office. They’ll evaluate the notes and translate them into code, whether for a scan, physical, or specific condition. Majorly, this role involves assessing and updating sensitive patient information. Thus, you must be accurate and careful with the data.
As with all medical positions, you will be expected to maintain confidentiality. Coders need to be aware of cybersecurity and what information they share.
Medical coding requires knowledge of multiple classification systems. There are three main types, with various subsections. Namely, coders must be familiar with ICD (international classification of diseases), CPT (current procedural terminology), and HCPCS (healthcare common procedure coding system). Each system is consistently updated to match new technologies, treatments, and the understanding and discovery of diseases.
Certain roles may also require knowledge of code sets such as NDC (national drug codes) and CDT (code on dental procedures and nomenclature).
Daily Responsibilities and Tasks
Day to day, coders evaluate dozens to hundreds of charts. The workload depends on the size and scope of the facility. Notably, major hospitals are the ones that often split billing and coding into two separate jobs. As a smaller clinic, many job postings will be for a single medical biller and coder role. Furthermore, you’re more likely to handle multiple departments at small institutions. If you work for a major hospital, you may be assigned to one single department.
Overall, to be successful in this role, you must be able to keep up with the workload. Hospitals often set an expectation of how many charts a coder evaluates each day. However, you will find some cases must take priority to ensure fast treatment for a patient. You will also come across charts that take a lot more time to code. Thus, you must know how to prioritize.
Additionally, as a coder, you may need to speak to hospital staff, such as doctors, billers, or administration. You may need to get clarity or more information. As a result, you should feel comfortable communicating with various individuals. Remember, as a medical coder, accuracy is key.
Salary
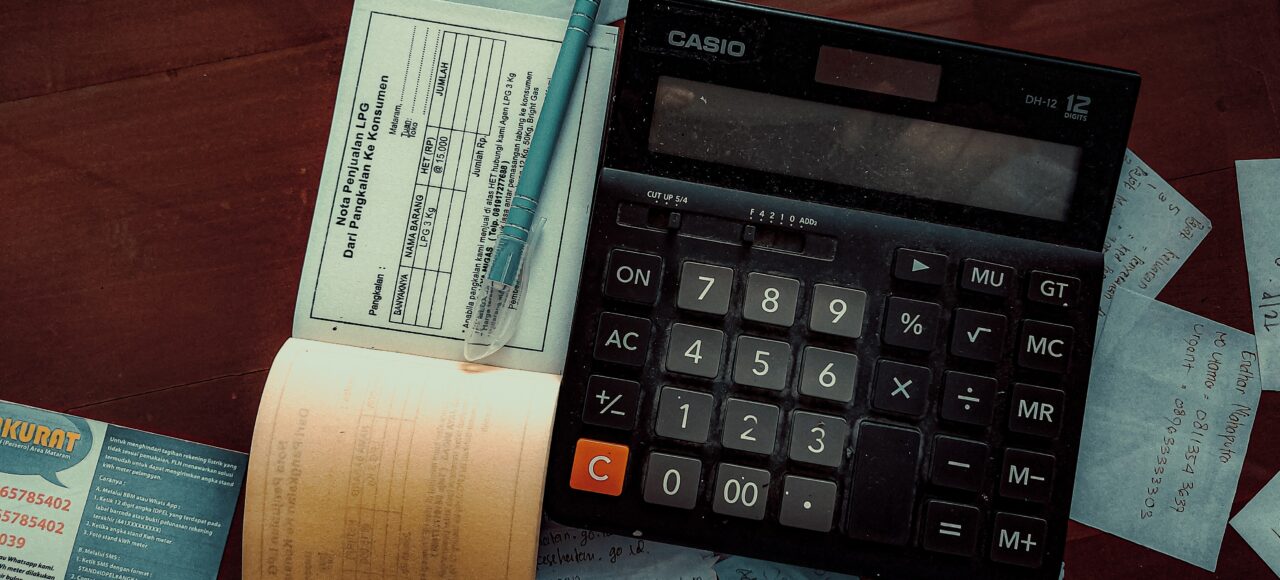
Medical coders earn a median salary of $53,051. This number can dip or rise depending on location and facility. Some areas report average pay closer to $35,000 annually, and others still provide a salary upwards of $60,000. Of course, larger hospitals are more likely to offer higher pay than smaller clinics.
As with many positions, you earn more with additional certifications and time. Thus, pursuing other credentials (such as the CIC, or certified inpatient coder) may help you improve your salary.
Medical Billing
Once coders are done with a chart, they hand it off to medical billers. At this end of the process, these professionals will communicate with insurance companies and follow up with payment. Billers also handle denied and rejected claims.
With rejections, they’ll deal with any errors and issues and resubmit the paperwork. Alternatively, a biller must communicate with the patient when something is denied. Medical billers may help the patient submit an appeal when dealing with claim denials. Notably, they do not handle this responsibility on their own.
Once a bill has gone through insurance, a biller must post any payment. However, a balance may still remain. In this case, medical billers will deal with the remaining amount in various ways. The patient may pay, the balance may be adjusted, or it’ll be written off entirely.
Daily Responsibilities and Tasks
Day to day, billers work with insurers, physicians and hospitals, and patients. They may communicate with many people over a single day. These communications may include resolving errors, explaining bills or coverage, and seeking clarification. As this job deals with collecting high fees and explaining denial of coverage, it can sometimes be stressful. Thus, medical billers need good communication and customer service skills.
Due to the sensitive nature of the role, medical billers must know how to create accurate claims. As a biller, you may submit dozens or hundreds of claims daily. Errors can delay payment to your facility or create unnecessary stress for the patient. Good attention to detail and editing skills ensure a quick and easy process.
Salary
Medical billers earn a median salary of $43,811. As with coding, this number can change with location and facility. You may see clinics paying around $35,000 or up to $60,000 annually. Again, larger hospitals are more likely to offer higher pay than smaller clinics.
As with many positions, you earn more with additional certifications and time. Thus, other credentials may help you improve your salary.

Education
Generally, hospitals and clinics will have the same standards for both medical coders and billers. What those standards are depends on the institution. Significantly, most facilities require that their coding and billing staff are certified. Some may also ask that new hires have an associate’s degree in a relevant field.
You can become certified by taking a course through a university or specialized training program. Then, you must take the certification exam.
There are many medical coding and billing programs available online and in-person. We recommend doing your research to find the best fit for you. Notably, you should ensure that the program is accredited. Unaccredited programs are not held to the same standards and may not be accepted by the certification exam board or an employer. Beyond that, you must decide if you have time to study on-campus or if you would prefer to work online.
Finally, consider if you only want to study medical billing or medical coding. This decision should be based on several factors, including your location. Indeed, would you be able to find a job as just a biller in your area? Or are local positions combined? Thankfully, some colleges offer medical billing and coding combo programs to help you expedite your education.
Final Thoughts
In addition to its accessible education requirements, medical billing or coding offers other benefits. Notably, there are many remote positions open in this field. Indeed, medical billing and coding was a remote opportunity before covid-19 sent us out of the office. Many professionals work from home because the tasks are completed 100% online. Some hospitals choose to hire independent contractors for this role. Thus, you can join this career as a full-time employee or a freelancer.
Additionally, the medical field is one of the more stable industries. As it constantly grows, more and more jobs are added each year. Indeed, medical billers and coders aren’t going anywhere anytime soon. These professionals are necessary to ensure accurate and timely payments for the sake of the patients and the medical providers.
Lakewood University
Lakewood University offers a variety of degree and certificate programs in the medical field. Notably, we provide medical billing, medical coding, and combination programs. Students can learn the fundamentals of both roles and prepare for the national certification exam. As a result, graduates will be fully prepared to get certified and begin their careers.
The medical billing program provides knowledge-based training and instruction on medical billing practices, EHR (electronic health record) data keeping, and insurance policies. On the other hand, the medical coding program covers CPT, HCPCS, and ICD-10-CM coding.
Interested in starting a career in medical billing or coding? Don’t hesitate – reach out to our admissions department today!